
Brown Dog Ticks and Repellents
Shujuan Li, Maureen Brophy, Dawn H. Gouge, Shaku Nair, Kathleen Walker.
University of Arizona
Brown Dog ticks vector (transmit) the bacteria that causes Rocky Mountain spotted fever (RMSF) in Arizona and northwest Mexico. RMSF is a serious disease that requires immediate medical attention and treatment.
Identification and life cycle
As its name suggests, the brown dog tick mainly feeds on the blood of dogs, but it will also feed on humans and other mammals. Brown dog ticks go through four life stages – egg, six-legged larva, eight-legged nymph, and adult. After hatching ticks must take a blood meal at every stage to survive. Between each stage, the tick sheds its exoskeleton and grows larger. Brown dog ticks are 3-host ticks and require a new host animal at each stage of their life.
Under warm conditions and with access to dogs, brown dog ticks can complete their entire life cycle in as little as two months. In locations that are warm year-round this tick can produce four generations each year. The tick usually spends its whole life in the host’s living area, which can lead to tick infestations inside homes, since dogs typically live some of their time with humans. Brown dog ticks can complete their entire life cycle indoors and reproduce year-round under these conditions.

Brown dog ticks Rhipicephalus sanguineus,
Photo by: William Nicholson (CDC)
How ticks find their hosts
Brown dog ticks can actively seek out hosts in the environment, using cues like carbon dioxide in exhaled breath, heat, and vibrations that cause the tick to run towards the host. They also use a strategy called “questing” where they wait ready to grasp onto an animal that brushes past.
Once a tick has found a host, it moves to a preferred feeding spot (often the ears and neck) and using its mouthparts the tick pierces the skin and continues to take a blood meal. Research has shown that brown dog ticks frequently group together when feeding on a host and the transfer of the bacteria that causes RMSF from infected to uninfected ticks can occur at this time.

Photo by: Jerry Butler, University of Florida
Once feeding is complete, the tick drops off the host and moves to a protective location in the environment to finish digestion and molt to the next life stage or lay eggs if the tick is a fertilized female.
Signs and symptoms of RMSF
Symptoms of RMSF appear 3-12 days after a bite from an infected tick, and include:
These symptoms are similar to other illnesses, and often people are unaware of having a recent tick bite. But it is important to seek medical attention as soon as possible, even if a symptomatic person has not been aware of being bitten by a tick.
Diagnosing RMSF is even more complicated in Sonora and other areas of Mexico because symptoms can be confused with other widespread illnesses, particularly dengue.
RMSF can be treated effectively with antibiotics, but early and complete treatment is critically important. RMSF can be deadly if it is not treated soon enough or if antibiotic treatment is discontinued prematurely. Based on the Centers for Disease Control and Prevention (CDC) guidelines, doxycycline should be prescribed and taken by the patient as soon as RMSF is suspected, and treatment should be continued for at least 72 hours after the fever subsides and until the patient improves.
Protect yourself and your family from tick bites by following some tick-tips:
1) Brown dog ticks spend most of their lives resting in protected places off their host. Reduce tick harborage opportunities by removing furniture, and unused items from under or around your home. Avoid using space under homes as storage areas and reduce plant growth next to and under your home. Wash pet bedding and vacuum inside homes weekly.

2) Check the whole family (including pets) for ticks daily, especially during the warmer months of the year. Remove ticks immediately using tweezers by grabbing them as close to the skin surface as possible and pulling straight off. Avoid squeezing ticks between your fingers!
3) In Arizona and Sonora, consider treating around your home for ticks spring-fall. Apply a pyrethroid pesticide (granular or liquid) around and under homes to reduce brown dog tick populations if they occur annually. Follow pesticide label instructions on how to apply products correctly. Use all recommended personal protective equipment including masks and gloves, application rates, buffer zones, and remove all outside toys and pet food and water containers before applying.
4) To treat your dog for ticks, you can use:
Wear gloves when applying tick treatments and follow label recommendations regarding how often you should repeat treatments.

5) When outdoors, wear long pants and sleeves and use an Environmental Protection Agency (EPA) registered tick repellent.
Seek medical advice if you or a family member become ill following a tick bite.
Note: To learn more about other ticks and tick-borne diseases, please watch: https://youtu.be/ZyAcJCbiXMA.
Repellents
Personal repellents are substances applied to skin, clothing, or other surfaces to repel or discourage insects and other arthropods, such as ticks, from feeding on humans. They include spray, lotion, and disposable towelette products and devices that can be worn or placed in an area to repel biting pests.
Mosquitoes and ticks are medically significant pests, some of which transmit disease-causing pathogens. Using repellents is one of the most effective ways to avoid bites outdoors.

In addition, repellents can be used to reduce bites from fleas, chiggers, biting midges (no-see-ums) and other blood-feeding arthropods. Repellents are EPA registered pesticides available in differing concentrations and rated to repel ticks and/or insects for specific lengths of time. Check product labels for the specifics before venturing outdoors and use the EPA search tool to find the ideal option for you: https://www.epa.gov/insect-repellents/find-repellent-right-you#search%20tool.
There are many repellents available with bold claims about their effectiveness. EPA registered products using the following active ingredients provide reliable results when used according to label directions: DEET, Picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), 2-undecanone and nootkatone.
Nootkatone is a relatively new active ingredient discovered and developed by the CDC and registered by the EPA for use in insecticides and insect repellents. Nootkatone is responsible for the characteristic smell and taste of grapefruit and is widely used in the fragrance industry to make perfumes and colognes.

Important considerations when choosing a repellent:
1) What pests are you repelling?
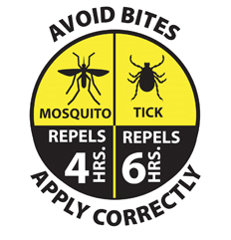
Look for the awareness graphic to determine the repellency time for mosquitoes or ticks.
2) Are you looking for a repellent to apply to skin, or to apply to clothing and equipment, such as a tent?
Never apply a repellent designed for fabrics to your skin. Using repellent and sunscreen products at the same time is an acceptable practice. When doing so, apply sunscreen first, followed by repellent.
3) Who is using the repellent?
Products are suitable for specific age groups. Read the product label carefully. Store repellents out of reach of children. Be aware that not all repellents are labeled for use on children. Very young children in carriers and strollers can be protected using mosquito netting while outdoors.

4) How long will you be outdoors?
Products are effective for specific lengths of time. However, extreme heat, sweating and water exposure will reduce the length of time a repellent is effective.
5) How abundant are the biting pests where you will be?
If you anticipate being in an area with high populations of ticks or mosquitoes, a repellent with a higher concentration of the active ingredient may be appropriate.
6) How and when should you apply your repellent?
Avoid applying repellents in enclosed areas. When outdoors, avoid inhaling repellent spray or applying repellents near food. Follow label recommendations regarding reapplication throughout time outdoors and reapply after swimming or sweating profusely.
7) Do not apply insect repellent to a child’s hands, or anyone’s eyes, mouth, ears, cuts, or irritated skin. Avoid using products containing OLE or PMD on children under 3 years of age.
8) Bites from triatomine bugs (also known as kissing or conenose bugs) can be reduced. When camping, apply permethrin around sleeping areas and on tents, and consider sleeping under bed nets.
9) Working or camping in locations with disease outbreaks involving arthropod vectors. Consider using permethrin-treated clothing and gear, or treat boots, external clothing and tents. Wash treated clothing before wearing them again.

Never apply permethrin directly to skin, the active ingredient will break down rapidly and can cause skin irritation.
10) Avoid covering repellent treated skin with clothing or going to bed before washing off the product. Remove repellent using gentle soap and water or cleansing wipes before covering up.
Be aware that most repellents are not effective against stinging arthropods like honey bees, wasps, ants, or scorpions.
Spatial repellent devices release a repellent into an area to create a “protective zone”. But few products have proven to be effective when tested by scientists. A study comparing various wearable devices and other repellents found that a wearable device emitting metofluthrin deterred Aedes aegypti mosquitoes (Rodriguez et al. 2017). The EPA does not review repellent devices. Spatial repellent devices should only be used outdoors.
Repellent wristbands and ultrasonic devices have not proven to be effective. Additionally, the effectiveness of outdoor candles, and coils is highly variable and depends largely on the active ingredients and specific design. Many product specific precautionary statements include instructions to avoid breathing vapors, washing hands thoroughly after handling and before eating, drinking, chewing gum, or using tobacco, removal and washing of contaminated clothing before reuse. Careful thought and selection is advisable.
Repellent safety
Read the entire product label before using a repellent. Even if you have used it before, read the label again - product directions change.
Follow the use directions carefully. Use only the amount directed, at the time and under the conditions specified, and for the purpose listed.
The CDC considers EPA-registered repellents safe for pregnant and nursing women if all registered product directions and precautions are followed.
Get specific information about repellents by contacting the National Pesticide Information Center 1-800-858-7378, or npic@ace.orst.edu or visit http://npic.orst.edu/ingred/ptype/repel.html.

If you, a child, or older dependent develops a rash or other reaction after using a repellent, stop using the repellent, wash the repellent off with mild soap and water.
If a person or pet eats or drinks a repellent call the poison control immediately.

Citation
Rodriguez SD, Chung H-N, Gonzales KK, Vulcan J, Li Y, Ahumada JA, Romero HM, De La Torre M, Shu F, and Hansen IA. 2017. Efficacy of some wearable devices compared with spray-on insect repellents for the yellow fever mosquito, Aedes aegypti (L.) (Diptera: Culicidae). Journal of Insect Science 17(1): 24; 1–6.
For more information on brown dog ticks and Rocky Mountain spotted fever: https://extension.arizona.edu/pubs/az1769-2018.pdf
For more information on repellents and vectors: https://extension.arizona.edu/pubs/az1761-2018.pdf
Vector Preparedness Virtual Workshop
The Vector Preparedness Virtual Workshop is a great opportunity for anyone with an interest in learning information on mosquito ID, surveillance, management and insecticide resistance in public health pests.
This workshop will present:
1) Basic aspects of mosquito biology and ecology, vector disease risks, and identification of a few important problematic mosquitoes in Arizona.
2) Basic information on integrated mosquito management.
3) Why it is important to trap mosquitoes, different types of traps that are available, and tips on how to use them.
4) Insecticide resistance, types of resistance (using bed bugs as examples), Integrated Pest Management (IPM), and public health pests IPM including bed bugs, head lice, German cockroaches, mosquitoes, flies, etc.
Arizona certified structural pesticide applicators can earn 4 CEUs from the AZ Department of Agriculture’s Pest Management Division (PMD) after completing the entire workshop. This course will be effective by August 30, 2021.
For more information on registration and workshop agenda, please contact Dr. Lucy Li, Associate in Extension - Public Health IPM, at lucyli@email.arizona.edu at University of Arizona.
Commensal Rodent Distribution Survey
The Southern California Urban Rodent Research Initiative (SCURRI) is a project researching urban rodent ecology and disease, their management, and the impact the management of rodents has on the environment.
Current roof rat range maps are out of date. In conjunction with the University of Arizona and Utah State University, University of California Agriculture and Natural Resources (UC ANR) is aiming to update this out of date map in order to be able to provide pest management professionals with the educational materials and training that they need to effectively manage urban roof rat populations.
This commensal rodent distribution survey has been created to help better understand the current distribution of the roof rat (Rattus rattus) in the United States. The information you provide will be used to help inform researchers of trends in urban rodent management. Participation is voluntary.
The survey can be found here at https://survey123.arcgis.com/share/907963bdd9da4b17b285edd20fce6952 or through the project website which has a much shorter link at https://www.ucscurri.com/ratsurvey
If you require more information about this survey please contact Human-Wildlife Interactions Advisor Dr. Niamh Quinn at nmquinn@ucanr.edu at University of California Cooperative Extension, Orange County.

School IPM in the COVID Era and Global Weed IPM are September's Featured Topics in the Western IPM Center IPM Hour
We have two timely topic coming up in this month's IPM Hour. Participate live on Wednesday, September 9, at noon Pacific. https://ucanr.zoom.us/j/97284412990
This month's presentations are:
Schools in the Time of COVID – More Questions than Answers
Description: An overview about situations faced in schools around the country as they reopened after lockdowns, and a brief discussion regarding disinfection, products, equipment and practices - as well as some helpful resources.
Presenter: Shaku Nair, University of Arizona
A Developing and Developed Countries Perspective on Implementation of Integrated Weed Management
Description: Concepts of integrated weed management with examples from South Asia and the United States, including social and economic issues.
Presenter: Anil Shrestha, California State University, Fresno
Check out upcoming Integrated Pest Management Webinars at https://www.epa.gov/managing-pests-schools/upcoming-integrated-pest-management-webinars
For more information about the EPA Schools program: http://www.epa.gov/schools/.
To view all our previous newsletters, visit: https://acis.cals.arizona.edu/community-ipm/home-and-school-ipm-newsletters
Acknowledgements
This material is in part funded by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award number 2017-70006-27145 that provides Extension IPM funding to the University of Arizona. Information regarding this document is within the guidelines of the Border 2020 Program funded by the U.S. Environmental Agency (EPA) and administered by NADB. Additional support is provided by the U.A. – Arizona Pest Management Center.
